MIT News搬运中英双语:Making sense of cell fate(理解细胞命运)
ENGLISH:
MIT researchers find timing and dosage of DNA-damaging drugs are key to whether a cancer cell dies or enters senescence.
Koch Institute
Publication Date:
July 27, 2023
Despite the proliferation of novel therapies such as immunotherapy or targeted therapies, radiation and chemotherapy remain the frontline treatment for cancer patients. About half of all patients still receive radiation and 60-80 percent receive chemotherapy.
Both radiation and chemotherapy work by damaging DNA, taking advantage of a vulnerability specific to cancer cells. Healthy cells are more likely to survive radiation and chemotherapy since their mechanisms for identifying and repairing DNA damage are intact. In cancer cells, these repair mechanisms are compromised by mutations. When cancer cells cannot adequately respond to the DNA damage caused by radiation and chemotherapy, ideally, they undergo apoptosis or die by other means.
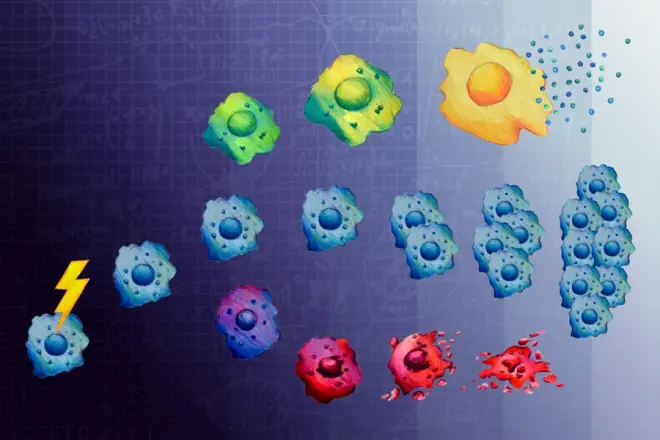
However, there is another fate for cells after DNA damage: senescence — a state where cells survive, but stop dividing. Senescent cells’ DNA has not been damaged enough to induce apoptosis but is too damaged to support cell division. While senescent cancer cells themselves are unable to proliferate and spread, they are bad actors in the fight against cancer because they seem to enable other cancer cells to develop more aggressively. Although a cancer cell’s fate is not apparent until a few days after treatment, the decision to survive, die, or enter senescence is made much earlier. But, precisely when and how that decision is made has not been well understood.
In a study of ovarian and osteosarcoma cancer cells appearing July 19 in Cell Systems, MIT researchers show that cell signaling proteins commonly associated with cell proliferation and apoptosis instead commit cancer cells to senescence within 12 hours of treatment with low doses of certain kinds of chemotherapy.
“When it comes to treating cancer, this study underscores that it’s important not to think too linearly about cell signaling,” says Michael Yaffe, who is a David H. Koch Professor of Science at MIT, the director of the MIT Center for Precision Cancer Medicine, a member of MIT’s Koch Institute for Integrative Cancer Research, and the senior author of the study. “If you assume that a particular treatment will always affect cancer cell signaling in the same way — you may be setting yourself up for many surprises, and treating cancers with the wrong combination of drugs.”
Using a combination of experiments with cancer cells and computational modeling, the team investigated the cell signaling mechanisms that prompt cancer cells to enter senescence after treatment with a commonly used anti-cancer agent. Their efforts singled out two protein kinases and a component of the AP-1 transcription factor complex as highly associated with the induction of senescence after DNA damage, despite the well-established roles for all of these molecules in promoting cell proliferation in cancer.
The researchers treated cancer cells with low and high doses of doxorubicin, a chemotherapy that interferes with the function with topoisomerase II, an enzyme that breaks and then repairs DNA strands during replication to fix tangles and other topological problems.
By measuring the effects of DNA damage on single cells at several time points ranging from six hours to four days after the initial exposure, the team created two datasets. In one dataset, the researchers tracked cell fate over time. For the second set, researchers measured relative cell signaling activity levels across a variety of proteins associated with responses to DNA damage or cellular stress, determination of cell fate, and progress through cell growth and division.
The two datasets were used to build a computational model that identifies correlations between time, dosage, signal, and cell fate. The model identified the activities of the MAP kinases Erk and JNK, and the transcription factor c-Jun as key components of the AP-1 protein likewise understood to involved in the induction of senescence. The researchers then validated these computational findings by showing that inhibition of JNK and Erk after DNA damage successfully prevented cells from entering senescence.
The researchers leveraged JNK and Erk inhibition to pinpoint exactly when cells made the decision to enter senescence. Surprisingly, they found that the decision to enter senescence was made within 12 hours of DNA damage, even though it took days to actually see the senescent cells accumulate. The team also found that with the passage of more time, these MAP kinases took on a different function: promoting the secretion of proinflammatory proteins called cytokines that are responsible for making other cancer cells proliferate and develop resistance to chemotherapy.
“Proteins like cytokines encourage ‘bad behavior’ in neighboring tumor cells that lead to more aggressive cancer progression,” says Tatiana Netterfield, a graduate student in the Yaffe lab and the lead author of the study. “Because of this, it is thought that senescent cells that stay near the tumor for long periods of time are detrimental to treating cancer.”
This study’s findings apply to cancer cells treated with a commonly used type of chemotherapy that stalls DNA replication after repair. But more broadly, the study emphasizes that “when treating cancer, it’s extremely important to understand the molecular characteristics of cancer cells and the contextual factors such as time and dosing that determine cell fate,” explains Netterfield.
The study, however, has more immediate implications for treatments that are already in use. One class of Erk inhibitors, MEK inhibitors, are used in the clinic with the expectation that they will curb cancer growth.
“We must be cautious about administering MEK inhibitors together with chemotherapies,” says Yaffe. “The combination may have the unintended effect of driving cells into proliferation, rather than senescence.”
In future work, the team will perform studies to understand how and why individual cells choose to proliferate instead of enter senescence. Additionally, the team is employing next-generation sequencing to understand which genes c-Jun is regulating in order to push cells toward senescence.
This study was funded, in part, by the Charles and Marjorie Holloway Foundation and the MIT Center for Precision Cancer Medicine.
汉:
麻省理工学院的研究人员发现,DNA损伤药物的时间和剂量是癌症细胞死亡或衰老的关键。
Bendta Schroeder |科赫研究所
出版日期:
2023年7月27日
尽管免疫疗法或靶向疗法等新疗法激增,但放射和化疗仍然是癌症患者的一线治疗。大约一半的患者仍在接受放射治疗,60-80%的患者接受化疗。
辐射和化疗都是通过破坏DNA发挥作用,利用癌症细胞特有的脆弱性。健康细胞更有可能在辐射和化疗中存活,因为它们识别和修复DNA损伤的机制是完整的。在癌症细胞中,这些修复机制受到突变的损害。当癌症细胞不能充分应对辐射和化疗引起的DNA损伤时,理想情况下,它们会发生凋亡或通过其他方式死亡。
然而,DNA损伤后的细胞还有另一种命运:衰老——细胞存活但停止分裂的状态。衰老细胞的DNA没有受到足够的损伤来诱导细胞凋亡,但损伤过大,无法支持细胞分裂。虽然衰老的癌症细胞本身无法增殖和扩散,但它们在对抗癌症的斗争中起着不良作用,因为它们似乎能使其他癌症细胞更积极地发育。尽管癌症细胞的命运在治疗后几天才明显,但存活、死亡或衰老的决定要早得多。但是,具体何时以及如何做出这一决定还没有得到很好的理解。
麻省理工学院的研究人员对7月19日出现在《细胞系统》杂志上的卵巢和骨肉瘤癌症细胞进行了一项研究,研究表明,通常与细胞增殖和凋亡相关的细胞信号蛋白会使癌症细胞在接受低剂量某些化学疗法治疗后12小时内衰老。
“在治疗癌症方面,这项研究强调,重要的是不要过于线性地思考细胞信号,”麻省理工学院大卫·H·科赫科学教授、麻省理工癌症精准医学中心主任、麻省理理工学院科赫综合癌症研究所成员、该研究的高级作者Michael Yaffe说。“如果你认为一种特定的治疗方法总是以同样的方式影响癌症细胞的信号传导,你可能会让自己陷入许多意外,并用错误的药物组合治疗癌症。”
“在治疗癌症方面,这项研究强调,重要的是不要过于线性地思考细胞信号,”麻省理工学院大卫·H·科赫科学教授、麻省理工癌症精准医学中心主任、麻省理理工学院科赫综合癌症研究所成员、该研究的高级作者Michael Yaffe说。“如果你认为一种特定的治疗方法总是以同样的方式影响癌症细胞的信号传导,你可能会让自己陷入许多意外,并用错误的药物组合治疗癌症。”
研究人员用低剂量和高剂量的阿霉素治疗癌症细胞,阿霉素是一种干扰拓扑异构酶II功能的化学疗法,这种酶在复制过程中断裂并修复DNA链,以修复缠结和其他拓扑问题。
通过在最初暴露后6小时至4天的几个时间点测量DNA损伤对单个细胞的影响,该团队创建了两个数据集。在一个数据集中,研究人员追踪了细胞随时间的命运。在第二组中,研究人员测量了各种蛋白质的相对细胞信号活性水平,这些蛋白质与对DNA损伤或细胞应激的反应、细胞命运的确定以及细胞生长和分裂的进展有关。
这两个数据集用于建立一个计算模型,确定时间、剂量、信号和细胞命运之间的相关性。该模型确定MAP激酶Erk和JNK以及转录因子c-Jun的活性是AP-1蛋白的关键成分,同样被认为参与衰老的诱导。研究人员随后验证了这些计算结果,表明DNA损伤后对JNK和Erk的抑制成功地阻止了细胞进入衰老。
雅菲实验室的研究生、该研究的主要作者Tatiana Netterfield说:“细胞因子等蛋白质会促进邻近肿瘤细胞的‘不良行为’,从而导致更具攻击性的癌症进展。”。“正因为如此,人们认为衰老细胞长时间停留在肿瘤附近对治疗癌症是有害的。”
这项研究的结果适用于用一种常用的化疗方法治疗的癌症细胞,这种化疗可以阻止修复后的DNA复制。但更广泛地说,该研究强调,“在治疗癌症时,了解癌症细胞的分子特征以及决定细胞命运的时间和剂量等背景因素极其重要,”Netterfield解释道。
然而,这项研究对已经在使用的治疗方法有更直接的影响。临床上使用了一类Erk抑制剂,即MEK抑制剂,预计它们将抑制癌症的生长。
Yaffe说:“我们必须谨慎使用MEK抑制剂和化疗。”。“这种组合可能会产生意想不到的效果,促使细胞增殖,而不是衰老。”。
在未来的工作中,该团队将进行研究,以了解单个细胞是如何以及为什么选择增殖而不是衰老的。此外,该团队正在使用下一代测序来了解c-Jun正在调节哪些基因,以推动细胞衰老。
这项研究部分由Charles和Marjorie Holloway基金会以及麻省理工学院癌症精准医学中心资助。
原网址:https://news.mit.edu/2023/making-sense-cell-fate-0727

